
This feature may help us to know how the pandemic affected patients who visited ED for psychiatric help. However, unlike in most other countries, a slack period occurred between the two peaks, when people in Taiwan could have relatively normal lives.
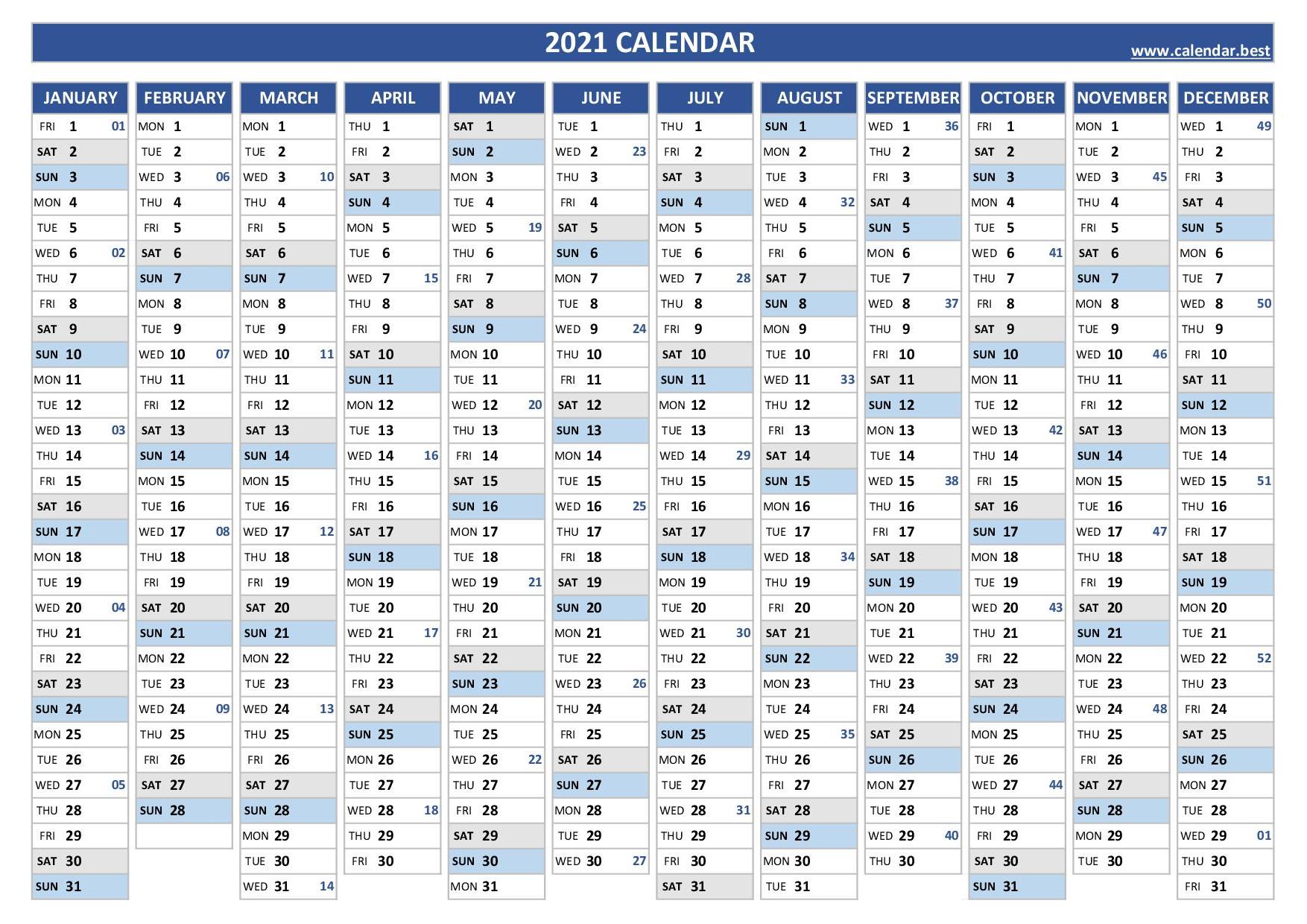
The second epidemic peak was from May 19, 2021, to July 26, 2021, and was a national level-3 epidemic. The first one was from January 20, 2020, when the first case of COVID-19 was detected, to June 7, 2020, when local restrictions eased. In Taiwan, two COVID-19 epidemic peaks occurred locally. This phenomenon indicated that people who sought psychiatric consultation in EDs during the COVID-19 peak period may be different from those in the pre-COVID-19 era. Compared with the baseline period of 2018–2019, a high proportion of patients with anxiety disorders, personality disorders, psychosis, and posttraumatic stress disorders visited EDs in 2020, while a decreased proportion of adjustment disorder was noted at the same time. Furthermore, the characteristics of people visiting psychiatric EDs have changed. Studies have revealed an approximately 30% decrease in psychiatric ED visits during the pandemic. However, the fear of COVID-19 may keep people with mental health problems from seeking help from an ED. A recent review suggested that this effect is contributed to by psychological, social and populational, and biological factors. The COVID-19 pandemic can affect people’s mental health in many aspects. Many possible factors might have contributed to decreased ED visits, but one hypothesis is that people would have avoided ED visits because of the fear of being infected by the COVID-19 virus. ED visits decreased significantly during the COVID-19 epidemic peak in Taiwan. This trend of ED visit reduction during the epidemic was observed in Taiwan in 2003, where the severe acute respiratory syndrome epidemic caused a 51.6% reduction in ED visits. In the United States, daily visits to emergency departments (EDs) of all causes decreased by approximately 50% across different states. The coronavirus disease 2019 (COVID-19) pandemic prominently changed people’s daily lives and health-seeking behaviors. This result raises the concern that mental health needs are masked during the pandemic. This study found that UPCs changed throughout the pandemic.

We observed significantly few men (34.9% vs 45.2%) and less violence (10.2% vs 17.6%) in the peak period compared with in the baseline period, but no significant difference was found compared with the slack period. ResultsĬompared with the baseline period, a significant decline in UPCs was observed in the pandemic peak period, and a rebound was observed in the slack period, with the median Q1, Q3 values of 22, 12 ), and 16, respectively. The total number of UPCs, patient demographic data such as sex and age of the patients seen, the referral system (whether police or emergency medical service or other sources), and the chief complaint (self-harm or violence) were recorded.
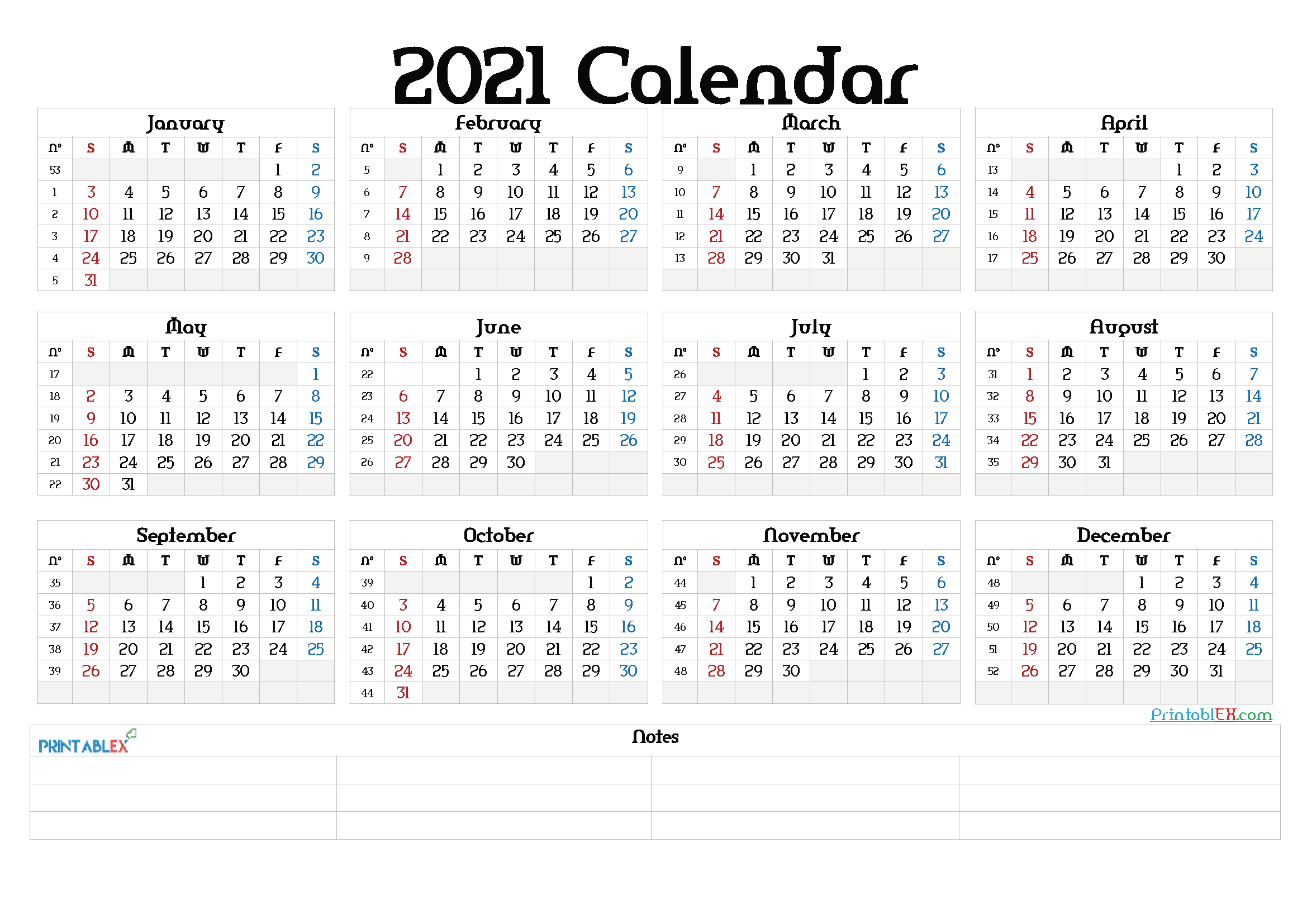
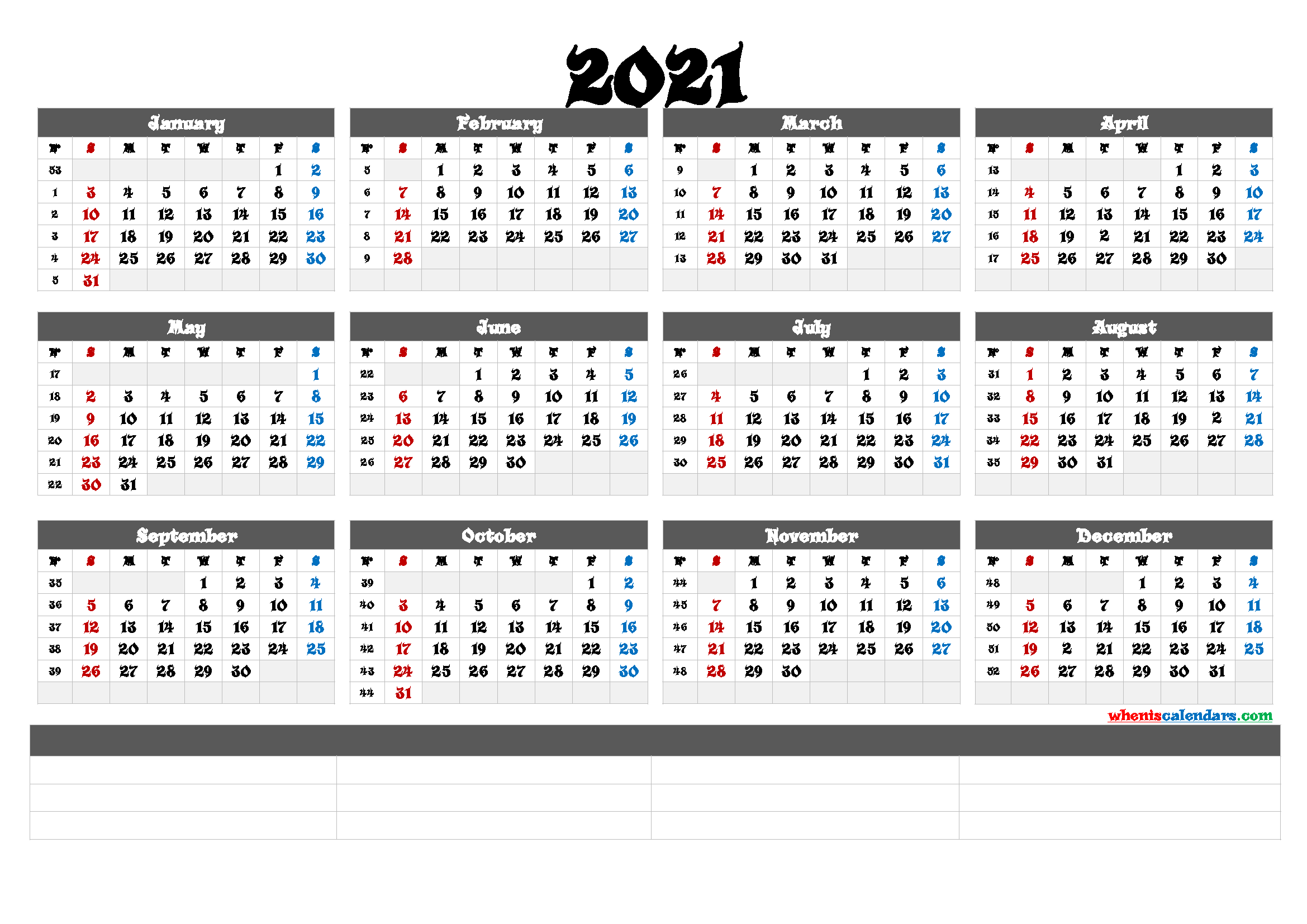
The corresponding baseline as calendar week 4–18, 2019, and the slack period as week 4–18, 2021. We defined the COVID-19 pandemic peak period as calendar week 4–18, 2020. This retrospective observational study evaluated UPCs in the ED of a referral medical center in Taiwan, where treated both physical and psychiatric complaints. Our study explored the changes in UPCs during and after the pandemic peak. The coronavirus disease 2019 pandemic significantly affected emergency department (ED) visits and urgent psychiatric consultation (UPC) seeking behavior in EDs.


 0 kommentar(er)
0 kommentar(er)
